There’s no single best medicine for diabetes. What works for one person might do little for another, or even cause side effects that make it worse. The truth is, diabetes treatment isn’t about finding the perfect pill-it’s about matching the right combination of medicines to your body, lifestyle, and health goals. And that’s something no one-size-fits-all list can give you.
How diabetes meds actually work
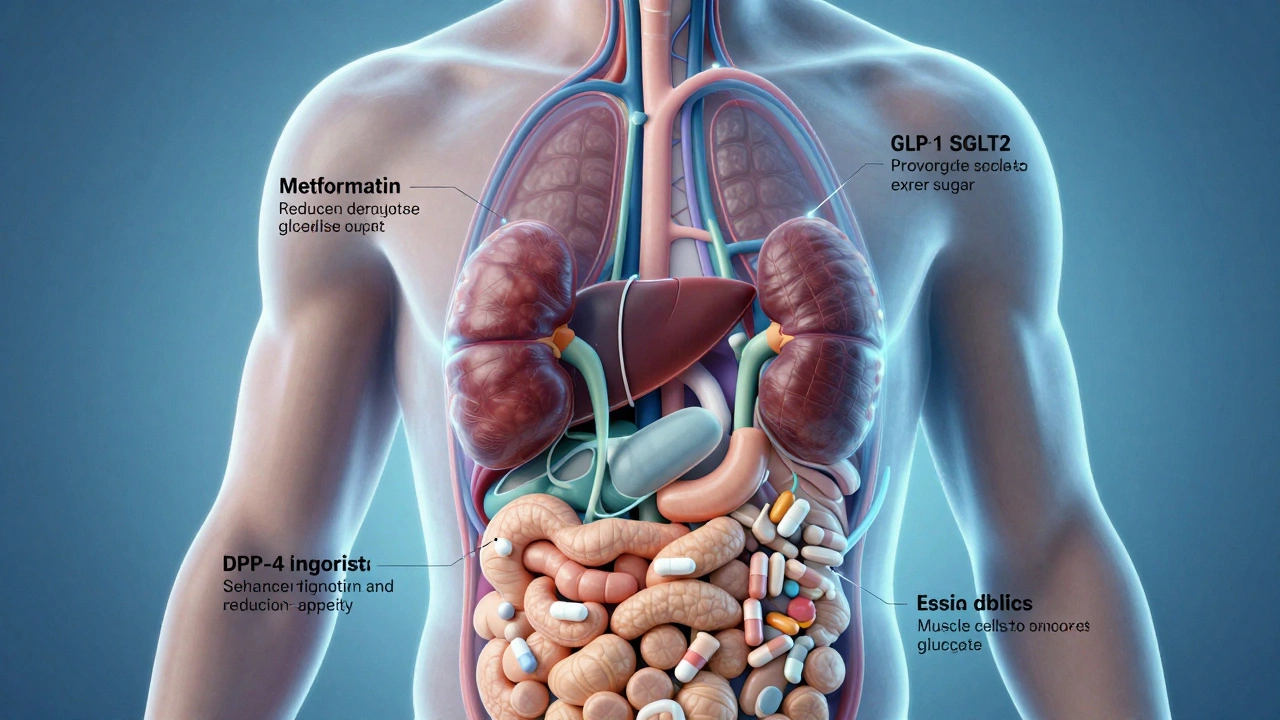
Not all diabetes medicines do the same thing. Some help your body use insulin better. Others make your pancreas pump out more insulin. Some slow down how fast your stomach digests carbs. A few even tell your kidneys to flush out extra sugar through urine. Knowing how each type works helps you understand why your doctor might pick one over another.
For example, metformin is usually the first choice for type 2 diabetes. It doesn’t make your body produce more insulin. Instead, it makes your liver stop dumping out so much glucose and helps your muscles absorb sugar more efficiently. It’s been used for over 60 years, is cheap, and has solid proof it lowers heart risks. About 70% of people with type 2 diabetes in the U.S. take it.
But if metformin alone isn’t enough, or if you can’t tolerate it, your doctor might add another drug. That’s where things get more complex.
The top diabetes medicines in 2026
Here are the five most commonly prescribed classes of diabetes medications today, and what they’re really like to use.
- Metformin - The baseline. Low risk of low blood sugar. Can cause stomach upset at first, but that usually fades. Often helps with modest weight loss.
- SGLT2 inhibitors - Drugs like empagliflozin and dapagliflozin. They make your kidneys pee out sugar. This lowers blood sugar, helps with weight loss, and cuts heart failure risk by up to 30% in high-risk patients. Side effects? More yeast infections and dehydration if you don’t drink enough water.
- GLP-1 receptor agonists - Semaglutide (Ozempic, Wegovy), liraglutide, dulaglutide. These mimic a gut hormone that slows digestion, reduces appetite, and boosts insulin. They’re great for weight loss-people often drop 10-15% of body weight. Some need daily shots, others are weekly. Side effects: nausea, vomiting, constipation. Not for people with a history of thyroid cancer.
- DPP-4 inhibitors - Sitagliptin, linagliptin. Mild blood sugar control. Weight neutral. Few side effects. But they don’t help much with weight or heart protection. Often added if other drugs aren’t enough.
- Insulin - Still the most powerful tool when your pancreas stops making enough. Comes in fast-acting, long-acting, or mixed forms. Requires careful dosing and frequent blood sugar checks. Can cause low blood sugar and weight gain. Often started when A1C stays above 9% despite other meds.
What doctors don’t always tell you
Many people assume that if their A1C is high, they just need a stronger drug. But that’s not always true. Sometimes the problem isn’t the medicine-it’s timing, diet, or stress.
A 2025 study in the Journal of the American Medical Association followed 1,200 people with type 2 diabetes who were on metformin but still had high blood sugar. Half were given a new drug. The other half got the same metformin dose but added weekly coaching on meal timing and walking after meals. After six months, the coaching group lowered their A1C just as much as the drug group-and lost more weight.
Medicine isn’t magic. It works best when it’s part of a plan. Skipping meals, drinking sugary coffee, or sleeping poorly can undo the effect of even the strongest drug.

When to think about insulin
Insulin gets a bad rap. People fear needles, weight gain, or the idea that they’ve "failed." But insulin isn’t a last resort-it’s a tool. If your pancreas has lost 70% or more of its insulin-making ability, no oral drug will fix that. Waiting too long to start insulin can damage your nerves, kidneys, and eyes.
Most people start with one daily injection of long-acting insulin, like glargine or detemir. It’s not complicated. Many use auto-injectors that feel like a quick pinch. Blood sugar checks go from 3 times a day to maybe once. And within weeks, energy levels often improve dramatically.
Insulin isn’t the end of the road. It’s often the start of better control.
What to avoid
There are no "miracle" diabetes cures. Supplements like cinnamon, berberine, or bitter melon may show tiny effects in lab studies, but they don’t replace proven medicines. The FDA has warned over 30 companies in the past year for selling fake diabetes products online.
Also avoid drugs that promise quick fixes. Some weight-loss pills sold as "natural" contain hidden, dangerous ingredients like sibutramine (banned since 2010) or phenolphthalein (a suspected carcinogen). These can cause heart attacks or liver damage.
Stick to medicines approved by the FDA or equivalent health agencies. If a drug isn’t on your doctor’s list, ask why.
Cost and access matter more than you think
Insulin used to cost $100 a vial. Now, in the U.S., many brands are capped at $35 per month thanks to the Inflation Reduction Act. That’s a game-changer. But not all insulins are covered equally. Some newer GLP-1 drugs like semaglutide can still cost $1,000 a month without insurance.
Ask your doctor about generic options. Metformin costs less than $5 a month. SGLT2 inhibitors have generics now too. If you’re paying too much, talk to your pharmacist. Many drugmakers have patient assistance programs. You don’t have to choose between medicine and rent.

It’s not about the best drug-it’s about the best fit
There’s no #1 best medicine for diabetes. The right one depends on:
- Are you trying to lose weight?
- Do you have heart or kidney disease?
- Can you handle daily shots?
- What’s your budget?
- Do you get dizzy when your blood sugar drops?
Your doctor doesn’t pick a drug because it’s the newest or the most expensive. They pick it because it fits your life. If you’re busy and hate pills, a weekly injection might be better than four daily ones. If you’re on a tight budget, metformin plus lifestyle changes might be all you need.
The goal isn’t to take the most drugs. It’s to keep your blood sugar in range without wrecking your day.
What happens if nothing seems to work?
If your A1C stays high after trying two or three different medicines, it’s time to look deeper. Maybe you have type 1 diabetes and were misdiagnosed as type 2. Maybe you have a rare form called MODY. Or maybe you’re taking a drug that interacts with another medicine you’re on-like steroids for arthritis or antidepressants.
Don’t give up. Ask for a referral to an endocrinologist. They specialize in hormone disorders and can run tests to find what’s really going on. Sometimes, a simple change-like switching from a drug that causes weight gain to one that helps you lose it-can turn things around.
Can I stop taking diabetes medicine if I lose weight?
Some people with type 2 diabetes can reduce or even stop meds after significant weight loss and improved fitness. Studies show that losing 10% of body weight can put diabetes into remission for some. But this doesn’t mean it’s cured. Blood sugar can creep back if weight returns. Always work with your doctor before stopping any medicine.
Which diabetes medicine causes the least side effects?
Metformin and DPP-4 inhibitors generally have the mildest side effect profiles. Metformin can cause bloating or diarrhea at first, but most people adjust. DPP-4 inhibitors rarely cause stomach issues or low blood sugar. But "least side effects" doesn’t mean "most effective." The best choice balances safety with results.
Is insulin better than pills?
Insulin is more powerful and works faster than pills, but it’s not "better"-it’s just different. Pills are easier for many people to take daily. Insulin is essential when the body can’t make enough on its own. The choice depends on your body’s needs, not which is "stronger."
Do diabetes medicines damage the kidneys?
Actually, some diabetes medicines protect the kidneys. SGLT2 inhibitors and GLP-1 agonists have been shown to slow kidney disease progression in people with diabetes. Metformin is safe unless kidney function is very low. Only older drugs like some sulfonylureas may need dose adjustments. Your doctor will check your kidney levels before prescribing.
Can I take over-the-counter supplements instead of prescription meds?
No. Supplements like chromium, alpha-lipoic acid, or herbal blends may claim to lower blood sugar, but none have proven results in large human trials. Some can interfere with your real meds or cause liver damage. The FDA doesn’t regulate supplements like drugs. Relying on them instead of proven treatment can lead to serious complications.
Next steps if you’re unsure
If you’re confused about which diabetes medicine is right for you, start here:
- Write down your biggest concerns: weight, cost, injections, side effects.
- Ask your doctor: "What’s the goal of this medicine? What happens if I don’t take it?"
- Request a referral to a certified diabetes care and education specialist (CDCES). They help you navigate meds, food, and daily habits.
- Don’t compare your treatment to someone else’s. Your diabetes is unique.
The best medicine for diabetes is the one you’ll actually take-consistently, safely, and without ruining your life. That’s the real goal.