If you think all heart surgeries are risky, you're not wrong—but there’s one that stands above the rest for sheer complexity: the heart transplant. Surgeons call it the Mount Everest of cardiac operations, and for good reason. Between timing, skill, and pressure, it doesn’t get tougher than this.
So why are heart transplants so demanding? First, there’s the clock—donor hearts can only survive a few hours outside the body, so every second counts. The surgeon isn’t just swapping out an old part for a new one; they’re racing against time while keeping the patient’s entire system stable. To make things even more nerve-wracking, the new heart has to snap into action fast in an environment that isn’t always welcoming.
But a transplant isn’t the only hard heart surgery out there. Procedures like the Ross procedure or some pediatric surgeries, where tiny hearts are involved, give even veteran doctors sweaty palms. Each adds its own twists, whether it's handling minuscule blood vessels or tackling multiple repairs at once.
- What Makes a Heart Surgery ‘Hard’?
- Heart Transplant: The Ultimate Challenge
- Other Contenders for the Toughest Spot
- What Patients and Families Should Know
- Tips for Facing Complex Heart Surgery
What Makes a Heart Surgery ‘Hard’?
Not every heart surgery is the same. Some are fairly routine and others are so tough they honestly keep surgeons up at night. But what makes a hardest heart surgery different from the rest? It boils down to a few factors.
- Time Pressure: Some heart surgeries, like transplants or certain emergency procedures, are a race against the clock. If parts of the heart or a donated organ don't get blood flow fast enough, they won’t work right.
- Precision: The heart’s packed with tiny, high-pressure blood vessels. Surgeons often work in spaces smaller than your pinky nail, and even a tiny slip can mean big trouble.
- Patient Condition: People who need the hardest surgeries are usually already in rough shape. Their heart may be failing or they've got other health problems that make things even riskier.
- unpredictability: Sometimes things change fast during surgery. A patient’s heart rhythm might crash or bleeding can get out of control within seconds. The surgical team has to adapt instantly.
To put this in perspective, here’s what success rates and typical challenges look like for different surgeries:
| Surgery Type | Average Success Rate | Common Challenges |
|---|---|---|
| Coronary Bypass | 98% | Blocked arteries, patient age, diabetes |
| Heart Valve Replacement | 95% | Loose tissue, infection, matching valve size |
| Pediatric Heart Defect Repair | 85-90% | Tiny anatomy, fragile patients |
| Heart Transplant | 80-85% | Organ rejection, timing, infection, weak patients |
Notice how the more complex the surgery and the tougher the patient’s situation, the lower the success rate drops—and the bigger the risks.
So, whether it’s stitching a paper-thin artery or swapping out a failing heart, what really makes a heart surgery hard is a combo of speed, steadiness, and the surgeon’s ability to handle the unknown. It’s not just skill with a scalpel, but full-on mental stamina.
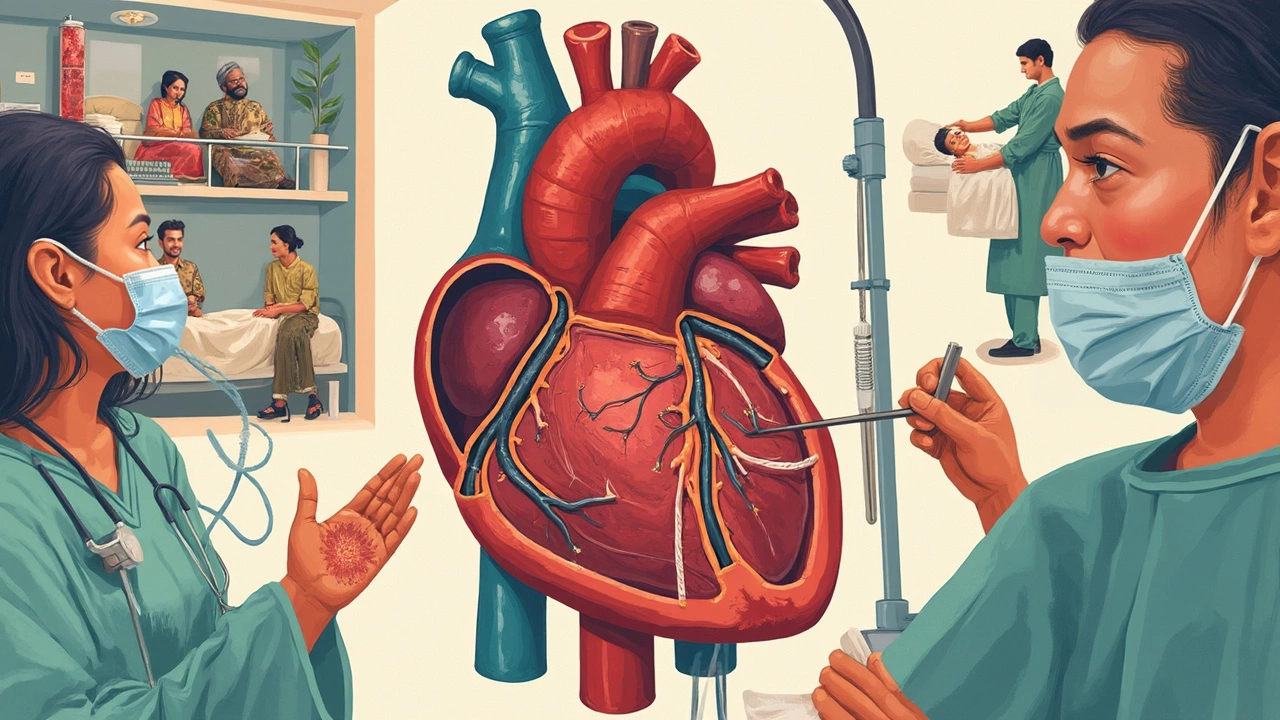
Heart Transplant: The Ultimate Challenge
The hardest heart surgery isn’t just another day in the OR—it’s the heart transplant. Every part of this surgery demands razor-sharp focus and skill, because lives hang in the balance. Basically, doctors replace a patient’s failing heart with a healthy one from a donor, but it’s not as simple as it sounds.
From the jump, timing is brutal. Surgeons have a window of about 4-6 hours once the donor heart is out. Any longer and the heart starts to lose its power. The rush starts before the first cut: the transplant team scrambles to get the heart to the hospital—sometimes hundreds of miles away—while the patient is kept on standby, ready to be wheeled in at any second.
During the surgery, the patient is hooked up to a heart-lung machine, which keeps blood and oxygen moving while their own heart is removed and the new one is stitched in. It’s a massive puzzle, lining up blood vessels perfectly to avoid leaks, clots, or blockage. One small slip could send things south in seconds.
Here’s what actually happens in a typical heart transplant:
- Patient arrives fasted and prepped; high risk, so extra tests before starting
- Anesthesia goes in, and they hook up the heart-lung machine
- Surgeons carefully take out the diseased heart
- Donor heart arrives—rushed, inspected, handled like a precious gadget
- Connecting blood vessels to new heart, making sure everything lines up
- Restart the new heart, cross fingers, monitor every signal on the screen
Because supply is short, only about 3,500 heart transplants happen each year across the world. The waitlist can be brutal, easily running into months or even a year. And survival rates show the risk: on average, about 85% of people make it through the first year, and just over half are still alive 10 years later. Take a quick look at the numbers:
| Stage | Typical Stat |
|---|---|
| Annual Worldwide Heart Transplants | ~3,500 |
| 1-Year Survival Rate | 85% |
| 5-Year Survival Rate | 70% |
| 10-Year Survival Rate | 50-55% |
Even after the surgery, things aren’t smooth sailing. Infection and organ rejection are common fears. Patients are loaded up on medicines to keep the immune system chill, but those same meds can lead to other complications. Watching for warning signs becomes part of daily life.
For families, it’s an emotional rollercoaster. You hope for the best, but you’re always bracing yourself. Knowing what to expect, and talking often with the care team, can make a big difference.
Other Contenders for the Toughest Spot
If you’re thinking heart transplant wins the "most intense surgery" trophy every year, take a look at these other giants in the world of hardest heart surgery. Some of these procedures have been known to keep even the most experienced surgeons up at night.
First up, the Ross procedure. It’s often the go-to for kids or young adults dealing with badly damaged aortic valves. Here, the surgeon removes the patient’s own healthy pulmonary valve and stitches it into the aortic spot, then puts a donor valve (or other replacement) in the pulmonary position. That’s a two-for-one deal packed into a single surgery, which means doubling the risk and the number of things that can go wrong. Surgeons have to do it all on a beating heart, with nerves of steel since the smallest slip can mean real trouble.
Next, take the Norwood procedure for newborns born with hypoplastic left heart syndrome. Imagine working on a heart smaller than a walnut, with vessels barely thicker than a thread. The whole surgery’s goal: convert a heart that's basically half-built into one that can actually support life. Death rates used to be sky-high, but thanks to surgical skill and medical advances, the odds have improved—still, it's among the riskiest and toughest in pediatrics.
- Valve replacement in adults with calcified valves—these are hearts that feel almost like rock. Surgeons actually have to chip and pry around calcium, sometimes for hours, to avoid ruptures or strokes.
- Aortic root surgery, where you’re rebuilding the main artery just where it leaves the heart. It’s right up against other vital arteries and the heart’s electrical system, so there’s zero room for error.
- Coronary artery bypass in patients with advanced diabetes, blockages everywhere, or who’ve had multiple surgeries. Scar tissue, fragile vessels, crazy anatomy—these cases test every skill in the book.
Check out this quick run-down of complication rates and average time on the operating table for a few of these tough procedures:
| Procedure | Average Surgery Time | Serious Complication Rate |
|---|---|---|
| Heart Transplant | 4-8 hours | Up to 30% |
| Ross Procedure | 6-10 hours | 15-20% |
| Norwood Procedure | 6-8 hours | 25-40% |
| Aortic Root Replacement | 5-7 hours | 10-15% |
| Coronary Bypass (complex) | 3-6 hours | 5-12% |
Each of these contenders brings a different flavor of challenge. Whether it’s juggling multiple repairs, handling delicate infant anatomy, or dealing with rock-hard valves, it’s not a job for the faint of heart.
What Patients and Families Should Know
Facing a hardest heart surgery like a heart transplant is overwhelming—not just for the patient, but for those close to them. Getting a handle on what to expect can ease some of the stress. Here are the key things you need to know before and after the big day.
First off, you don’t just get on the transplant list and then jump straight into surgery. There’s a waiting game involved, and it can be long. The match depends on blood type, body size, urgency, and, of course, availability of a donor heart. Some folks wait weeks, others months. In 2024, the average wait time for a heart in the U.S. was around 6 months, but it can change fast based on your health and the hospital's region.
Let’s talk about the surgery itself. A dedicated team—surgeons, nurses, anesthesiologists, and sometimes other specialists—work for hours. Most heart transplants take 4 to 6 hours. During this time, patients are under general anesthesia with machines doing the job of the heart and lungs. Family members sit it out in waiting rooms, praying for updates, but hospitals usually keep you posted step by step.
| Fact | Detail |
|---|---|
| Heart transplant surgery time | 4-6 hours (average) |
| Average hospital stay after transplant | 2-3 weeks |
| 1-year survival rate | 85-90% |
| Main risks | Organ rejection, infection, bleeding |
Recovery isn’t a sprint. After surgery, most people spend 2-3 weeks in the hospital, with at least a few days in intensive care. Around-the-clock monitoring is standard. What really surprises most people is the amount of blood tests, biopsies, and checkups you need. For the first year, you’ll have regular visits to make sure the new heart’s not being rejected. Immunosuppressant meds are for life, and they keep your body from fighting the new organ—but they also raise your risk of infections.
- Stick closely to the medication plan. Missing even a single dose can be risky.
- Learn the signs of rejection: fever, fatigue, weight gain, swelling, or shortness of breath.
- Keep a logbook of symptoms, meds, and questions for your care team.
- Family support is huge—have someone help with transport, meals, paperwork, and moral support.
One thing people often aren’t told: mental health after a tough surgery is just as important as physical healing. Lots of transplant centers offer counseling and support groups. It’s okay to lean on these resources, because the road can get bumpy. I remember Anjali feeling lost after a close friend had a major surgery—but talking to others who’d been there really helped them through. Don’t try to tough it out alone.
Tips for Facing Complex Heart Surgery
Walking into the hospital knowing you’re about to have a hardest heart surgery is pretty much the definition of stressful. But, the way you prep for it—mentally and physically—makes a difference in your outcome and your mindset. Here’s what people facing a heart transplant or any super tough heart procedure should keep in mind.
- Understand the procedure: Don’t just nod along while the doctor talks. Ask them to explain what’s actually going to happen—step by step if you have to. Knowledge really does help cut down on fear.
- Prep your body: Eat as healthy as your doctor allows, get a bit of movement in, and, if you smoke, quit ASAP. There’s solid proof your recovery goes much smoother if you come in as strong as you can—think of it as training for a marathon.
- Get your papers in order: This isn’t fun, but having your insurance, ID, and any healthcare directives sorted helps everyone—including you—focus on what matters most: your health.
- Line up your support: Whether it’s a spouse, family member, or friend, have someone who can help drive, ask questions, or even just sit with you before surgery. Emotional support goes further than people think. When my wife, Anjali, went through a scare with her heart, having a circle of care made every appointment easier to handle.
- Ask about infection prevention: Hospital infections aren’t some random risk—they’re real and sticking to protocols matters. Ask how your surgical team prevents them and what you can do (it’s usually handwashing, but sometimes there’s more).
The stats back up the value of good prep and support. Check out this quick breakdown from recent studies:
| Preparation Factor | Impact on Recovery/Complications |
|---|---|
| Stopping smoking 4+ weeks before surgery | Up to 50% lower rate of lung complications |
| Strong social support (care partner present) | 35% faster recovery time, fewer readmissions |
| Following post-op infection protocols | Reduces risk of surgical site infection by 60% |
After the surgery, listen to your doctors even when you start to feel normal. A lot of setbacks—like picking up something heavy too soon or skipping medication—happen when people get overconfident. One last thing: don’t be afraid to ask for help if you feel down afterward. Feeling blue after major surgery is common, and you’re not alone.
