Ozempic Weight Loss Estimator
This calculator estimates potential weight loss based on clinical data showing average results from Ozempic usage. Remember: results vary by individual and depend on lifestyle changes.
Your Information
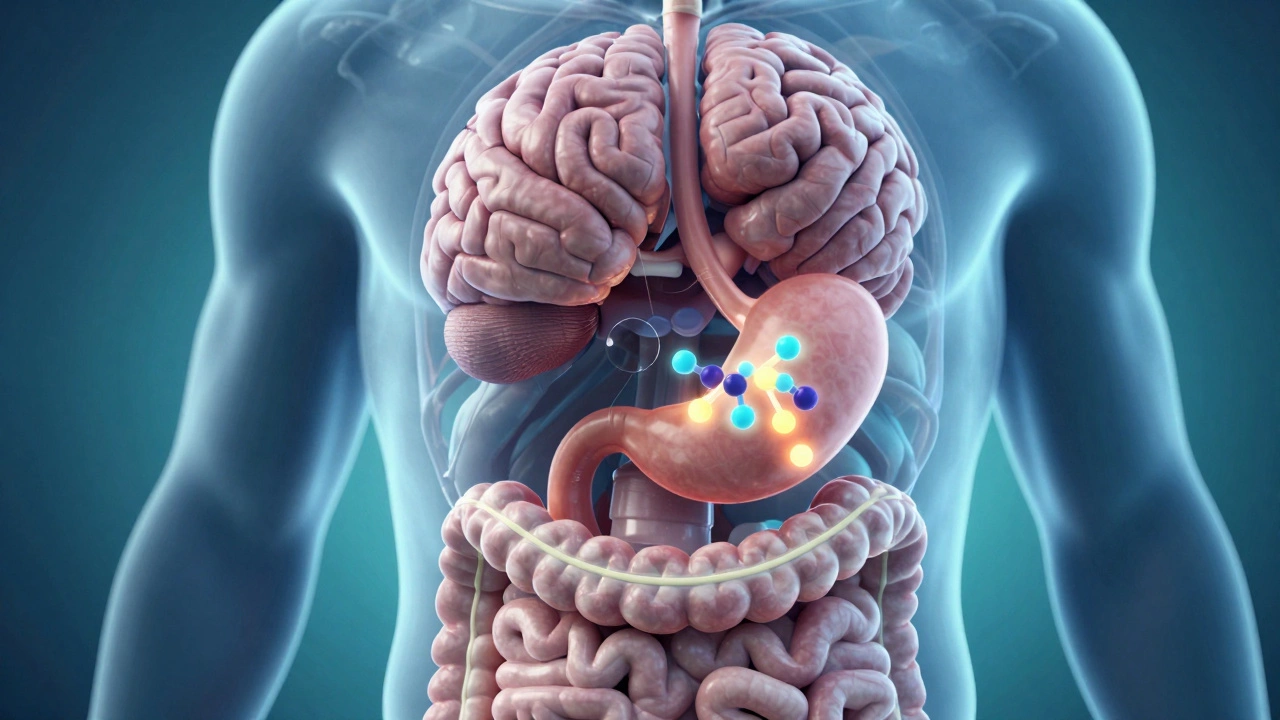
When people start asking how Ozempic works for weight loss, they’re not just curious-they’re looking for real answers. Ozempic isn’t a magic pill. It doesn’t burn fat overnight or trick your body into losing weight without effort. But it does something powerful: it changes how your brain and stomach talk to each other about food. And that’s why millions have seen real, lasting results.
What Ozempic Actually Is
Ozempic is the brand name for semaglutide, a drug originally developed to treat type 2 diabetes. Its main job was to help the body produce more insulin when blood sugar rises after eating. But doctors noticed something unexpected: patients on Ozempic kept losing weight-even when they didn’t try. That led to deeper research, and eventually, a higher-dose version called Wegovy was approved just for weight loss. But Ozempic itself is still widely used off-label for this purpose.
The active ingredient, semaglutide, is a GLP-1 receptor agonist. That’s a fancy way of saying it mimics a hormone your body already makes: glucagon-like peptide-1. This hormone is released after you eat, and it does three things: slows down stomach emptying, tells your pancreas to release insulin, and signals your brain that you’re full.
How It Slows Down Your Appetite
Most weight loss drugs try to boost metabolism or block fat absorption. Ozempic doesn’t do either. Instead, it works on your brain’s hunger center-the hypothalamus. When semaglutide binds to GLP-1 receptors there, it reduces cravings and makes you feel satisfied after smaller meals.
Think of it like turning down the volume on your hunger signal. You still feel hungry sometimes, but the urge to snack, reach for sweets, or overeat at dinner isn’t as loud. In clinical trials, people on Ozempic reported feeling full longer after meals and had fewer thoughts about food throughout the day. One study published in The New England Journal of Medicine showed that participants lost an average of 15% of their body weight over 68 weeks-without changing their diet or exercise habits dramatically.
It Slows Down Your Stomach
Have you ever eaten a big meal and felt bloated for hours? That’s your stomach taking its time to digest. Ozempic makes that process even slower. By delaying gastric emptying, food stays in your stomach longer. That means your blood sugar rises more gradually, and you don’t get those spikes and crashes that trigger cravings.
This effect isn’t just about feeling full. It also helps stabilize energy levels. People who used to crash after lunch or snack every afternoon often find those urges fade. The result? Fewer impulsive food choices and less overall calorie intake-not because they’re counting calories, but because their body’s natural signals are working better.
Why It Works Better Than Dieting Alone
Most diets fail because they rely on willpower. Willpower runs out. Hunger doesn’t. Ozempic doesn’t ask you to be stronger. It changes the biology behind the urge to eat.
When you cut calories, your body fights back. Leptin drops. Ghrelin rises. Your brain thinks you’re starving. That’s why people regain weight after dieting. Ozempic tricks your brain into thinking you’re not in danger. It lowers ghrelin (the hunger hormone) and keeps leptin (the fullness hormone) stable. That’s why weight loss with Ozempic tends to be more sustainable than with dieting alone.

Real Results, Real Time
People typically start noticing changes within the first few weeks. Appetite suppression kicks in around week two or three. By week six, many report eating smaller portions without feeling deprived. The biggest weight loss happens between months three and six. After that, progress slows-but doesn’t stop-unless they stop taking it.
In one real-world study tracking over 1,000 patients using Ozempic for weight loss, 72% lost at least 10% of their body weight within a year. About 40% lost over 15%. Those numbers are higher than most other weight loss medications. And unlike some older drugs, Ozempic doesn’t cause jitteriness, insomnia, or heart palpitations. It’s not stimulant-based. It works with your body’s natural systems.
Side Effects and Who Should Avoid It
It’s not without downsides. The most common side effects are nausea, vomiting, constipation, and diarrhea. These usually happen in the first few weeks as your body adjusts. Taking the dose slowly-starting low and increasing gradually-helps reduce them. Most people find these symptoms fade after a month or two.
Ozempic isn’t for everyone. People with a personal or family history of medullary thyroid cancer or multiple endocrine neoplasia syndrome type 2 should not use it. There’s a boxed warning from the FDA about thyroid tumors seen in animal studies, though no clear link has been found in humans. Pregnant women, people with severe digestive disorders like gastroparesis, or those with a history of pancreatitis should also avoid it.
It’s Not a Standalone Solution
Ozempic doesn’t replace healthy habits. It makes them easier. People who combine it with regular movement, protein-rich meals, and sleep hygiene lose more weight and keep it off longer. Those who take it and keep eating the same high-sugar, high-fat diet still gain weight-just slower.
The best outcomes come from people who use Ozempic as a tool, not a crutch. They learn to listen to their body again. They stop eating out of boredom or stress. They start choosing foods that keep them full longer. Ozempic gives them the space to rebuild their relationship with food.

What Happens When You Stop?
This is the biggest question people don’t ask until it’s too late. If you stop taking Ozempic, your appetite and stomach emptying return to normal. Most people regain some weight-often 20% to 30% of what they lost-within a year of stopping.
That doesn’t mean it didn’t work. It means the drug was managing a biological signal, not fixing the root cause. For many, that’s okay. They use it for 12 to 18 months to jumpstart weight loss, then transition to lifestyle changes to maintain. Others stay on it long-term if it’s affordable and well-tolerated.
There’s no shame in needing help. Obesity is a chronic disease, like high blood pressure or diabetes. Just as someone with hypertension takes medication daily, some people need ongoing support to manage their weight. Ozempic is one tool in that toolkit.
How It Compares to Other Weight Loss Drugs
There are other GLP-1 drugs like Saxenda (liraglutide) and Wegovy (higher-dose semaglutide). Wegovy is essentially the same drug as Ozempic, but at a higher dose approved specifically for weight loss. Ozempic is often used off-label because it’s cheaper and more accessible.
Compared to older drugs like phentermine or Contrave, Ozempic has fewer cardiovascular risks and doesn’t affect sleep or mood. Unlike Orlistat, which blocks fat absorption and causes oily stools, Ozempic doesn’t mess with digestion in a messy way. It’s generally better tolerated and more effective.
But it’s not the only option. Newer drugs like Mounjaro (tirzepatide) target both GLP-1 and GIP receptors and may lead to even greater weight loss. But they’re newer, more expensive, and harder to get.
Getting Started with Ozempic
You can’t buy Ozempic over the counter. It requires a prescription. Most people get it through a doctor who specializes in weight management, endocrinology, or metabolic health. Some weight loss clinics offer it as part of a broader program that includes nutrition counseling and behavioral support.
Before starting, your doctor will likely check your thyroid function, kidney health, and blood sugar levels. They’ll also ask about your medical history and any medications you’re taking. It’s not a quick fix, and it’s not for everyone-but for those who need it, it can be life-changing.
It’s not about becoming someone else. It’s about giving your body a chance to reset. Ozempic doesn’t change who you are. It just helps you eat less, feel better, and move more-with less internal resistance.
Can Ozempic be used for weight loss if I don’t have diabetes?
Yes. While Ozempic was originally approved for type 2 diabetes, doctors commonly prescribe it off-label for weight loss in people without diabetes. The same mechanism-slowing stomach emptying and reducing appetite-works regardless of blood sugar status. Many weight loss clinics now offer it as part of a comprehensive program for overweight or obese adults.
How long does it take to see weight loss with Ozempic?
Most people start noticing reduced hunger and smaller portion sizes within 2 to 4 weeks. Noticeable weight loss usually begins around week 6 to 8. The most significant loss happens between months 3 and 6. On average, people lose 10% to 15% of their body weight within a year when combined with lifestyle changes.
Is Ozempic better than diet and exercise alone?
For most people with obesity, diet and exercise alone aren’t enough long-term. Biology fights back-hunger hormones rise, metabolism slows. Ozempic helps override those signals. Studies show people using Ozempic lose significantly more weight than those relying only on lifestyle changes. It doesn’t replace healthy habits-it makes them sustainable.
What are the long-term risks of using Ozempic?
Long-term data beyond five years is still limited, but current evidence shows it’s generally safe for most people. The biggest concern is potential thyroid tumors seen in rodents, but no clear link exists in humans. Side effects like nausea and constipation usually improve over time. Regular monitoring by a doctor is recommended, especially if you have a history of pancreatitis, gallbladder disease, or kidney issues.
Can I drink alcohol while taking Ozempic?
Moderate alcohol is usually fine, but it’s not recommended. Alcohol can lower blood sugar, and since Ozempic also lowers blood sugar, the combination increases the risk of hypoglycemia. Alcohol can also trigger cravings and lead to overeating, which defeats the purpose. If you drink, do so sparingly and always eat something first.
Does Ozempic cause muscle loss?
Some weight loss from any method can include muscle loss, but Ozempic doesn’t specifically target muscle. Studies show that when combined with resistance training and adequate protein intake, people on Ozempic lose mostly fat, not muscle. To protect muscle, aim for 1.2 to 1.6 grams of protein per kilogram of body weight daily and include strength exercises at least twice a week.