Diabetes Treatment Comparison Tool
Your Health Profile
Tirzepatide Potential Benefits
Tirzepatide Benefits
Most EffectiveDiabetes treatment took a big step forward in 2024 with the arrival of a new class of drugs that don’t just lower blood sugar-they help you lose weight, protect your heart, and even reduce the risk of kidney damage. If you’ve been wondering what’s new in diabetes meds, the answer isn’t just one drug. It’s a shift in how we treat the disease entirely.
What’s Actually New in 2024?
The biggest news isn’t a brand-new molecule. It’s the expanded use of tirzepatide, the active ingredient in Mounjaro and Zepbound. Originally approved for type 2 diabetes under the brand name Mounjaro in 2022, it gained FDA approval for weight loss as Zepbound in late 2023. By 2024, doctors across the U.S., Europe, and India started prescribing it more widely-not just for obesity, but as a first-line treatment for people with type 2 diabetes who also struggle with weight.
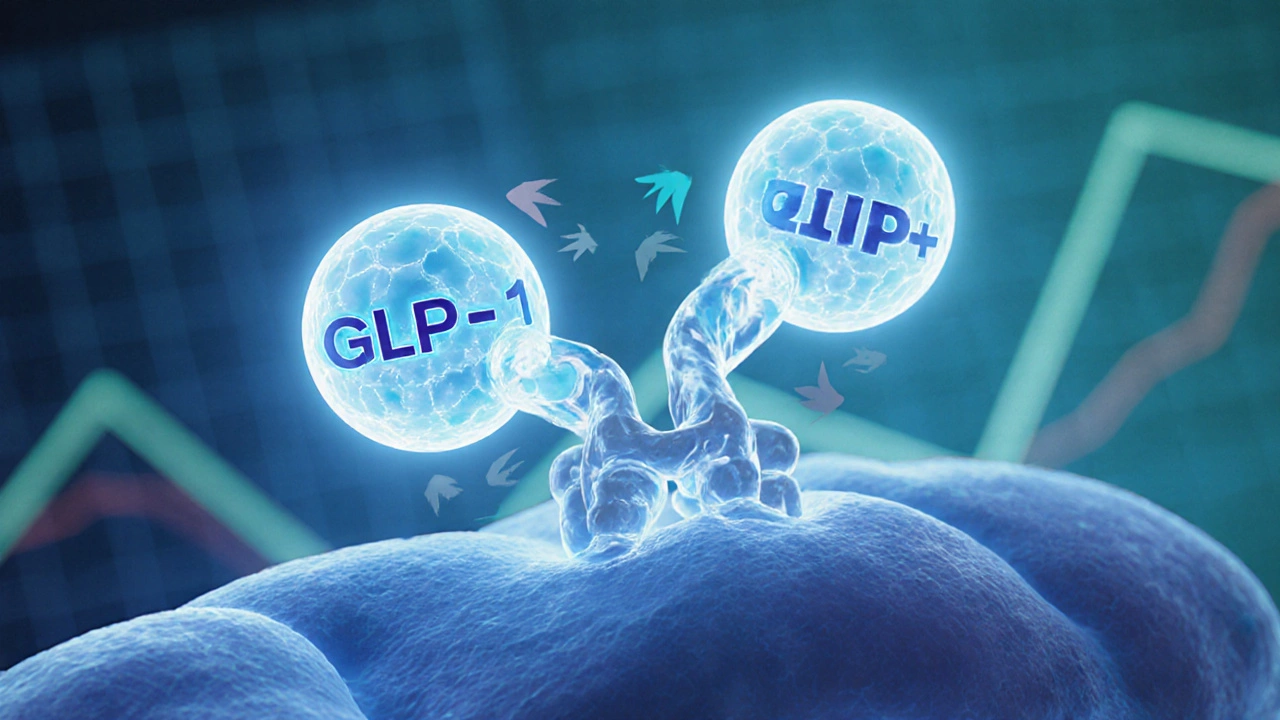
Unlike older drugs like metformin or sulfonylureas, tirzepatide works like a double-key lock. It mimics two natural hormones: GLP-1 and GIP. These hormones tell your pancreas to release insulin when blood sugar rises, slow down stomach emptying so you feel full longer, and reduce appetite signals to your brain. The result? People using tirzepatide lost an average of 15-20% of their body weight in clinical trials-far more than any previous diabetes drug.
How Does It Compare to Other Drugs?
Here’s how tirzepatide stacks up against other common diabetes medications:
| Drug Name | Active Ingredient | Weight Loss (Average) | Heart Protection | Cost (Monthly, USD) |
|---|---|---|---|---|
| Mounjaro / Zepbound | Tirzepatide | 15-20% | Yes | $1,000-$1,300 |
| Wegovy | Semaglutide | 10-15% | Yes | $1,100-$1,400 |
| Metformin | Metformin | 2-5% | Mild | $10-$30 |
| SGLT2 Inhibitors | Empagliflozin, Dapagliflozin | 5-8% | Yes | $400-$600 |
| Insulin | Insulin glargine, lispro | None or gain | No | $200-$800 |
What stands out? Tirzepatide isn’t just better at lowering blood sugar-it’s the only drug in this group that consistently delivers major weight loss while protecting the heart and kidneys. SGLT2 inhibitors like Jardiance and Farxiga also protect the heart and kidneys, but they don’t shrink waistlines as dramatically. And while semaglutide (Wegovy) is close, tirzepatide’s dual-action design gives it a slight edge in both weight loss and glucose control.
Who Should Consider It?
This isn’t for everyone. Tirzepatide is approved for adults with type 2 diabetes, especially those who:
- Have a BMI over 27 (overweight) or 30 (obese)
- Are struggling to control blood sugar with metformin alone
- Want to reduce or stop insulin use
- Have heart disease, high blood pressure, or early signs of kidney damage
It’s not approved for type 1 diabetes. People with a personal or family history of medullary thyroid cancer or multiple endocrine neoplasia syndrome type 2 should avoid it entirely-there’s a small risk of thyroid tumors in animal studies, though none have been confirmed in humans.
Many patients in India and Southeast Asia are now switching to tirzepatide after years of relying on metformin and insulin. One patient in Bangalore, a 58-year-old school teacher with 12 years of diabetes, stopped insulin after three months on tirzepatide. Her HbA1c dropped from 8.9% to 6.2%. She lost 24 kg and no longer feels tired after meals.

Side Effects and Real-World Challenges
Like all medications, tirzepatide has downsides. The most common are nausea, vomiting, diarrhea, and constipation-especially when starting or increasing the dose. These usually fade after 4-6 weeks. About 1 in 10 people stop taking it because of gut issues.
Another problem? Cost. In the U.S., it’s expensive. In India, it’s not yet widely available through public health programs. Most patients pay out-of-pocket or rely on private insurance. A single pen costs ₹8,000-₹11,000, and you need one every week. That’s more than most people can afford without financial planning.
Doctors are starting to offer patient assistance programs and generic alternatives are expected to arrive in 2026. Until then, many are using lower doses (5 mg or 7 mg) to reduce side effects and cost while still getting benefits.
What’s Next After 2024?
The next wave of diabetes drugs is already in trials. Oral versions of GLP-1/GIP drugs are coming-no injections needed. Eli Lilly and Novo Nordisk are testing pills that work just like tirzepatide but can be swallowed. Early results show promise, with blood sugar control matching injections.
Researchers are also exploring triple-agonist drugs that mimic GLP-1, GIP, and glucagon. These could offer even more weight loss and better blood sugar control. One experimental drug, retatrutide, is showing 25%+ weight loss in early trials. It’s not approved yet, but if it passes Phase 3, it could be the next big thing by 2026.

Is This the End of Insulin?
No. Insulin is still vital for people with advanced diabetes, type 1 diabetes, or those who can’t tolerate GLP-1 drugs. But for many with type 2 diabetes, insulin is no longer the first choice. Tirzepatide is changing the game. It’s not a miracle cure-but it’s the closest thing we’ve had in decades to a treatment that fixes multiple problems at once: high blood sugar, excess weight, and rising heart risk.
If you’ve been told you need insulin, ask your doctor if tirzepatide might be an option. Bring your recent HbA1c, weight history, and any heart or kidney test results. Don’t assume insulin is your only path. The treatment landscape has changed-and you deserve to know what’s possible now.
Is tirzepatide the same as semaglutide?
No. Tirzepatide (Mounjaro, Zepbound) mimics two hormones-GLP-1 and GIP-while semaglutide (Wegovy, Ozempic) only mimics GLP-1. This dual action makes tirzepatide more effective at lowering blood sugar and promoting weight loss in most studies. People on tirzepatide typically lose 2-5% more weight than those on semaglutide.
Can I take tirzepatide if I have kidney problems?
Yes, and in fact, it’s often recommended. Tirzepatide has been shown to slow the progression of kidney disease in people with type 2 diabetes. It reduces protein in the urine and lowers the risk of needing dialysis. However, your doctor will check your kidney function before starting and may adjust the dose if your kidneys are already severely damaged.
How long does it take to see results?
Most people notice reduced hunger and better blood sugar control within the first 2-4 weeks. Weight loss starts slowly but becomes noticeable after 8-12 weeks. The full benefits-like improved heart health and kidney protection-build over 6-12 months. Consistency matters more than speed.
Does tirzepatide cause low blood sugar?
Not usually on its own. Unlike insulin or sulfonylureas, tirzepatide only triggers insulin release when blood sugar is high. That means it rarely causes dangerous lows. But if you’re taking it with insulin or sulfonylureas, your risk increases. Your doctor will likely lower those other doses when you start tirzepatide.
Is there a generic version of tirzepatide available?
No, not yet. Tirzepatide is still under patent protection. Generic versions are expected to arrive in 2026 or later. Until then, some patients use lower doses (like 5 mg instead of 10 mg or 15 mg) to stretch their supply and reduce cost. Always consult your doctor before adjusting your dose.
What Should You Do Now?
If you have type 2 diabetes and aren’t at your target HbA1c-or if you’re gaining weight despite taking medication-it’s time to ask about tirzepatide. Bring your latest lab reports, a list of all current meds, and your weight history to your next appointment. Ask: “Is tirzepatide right for me? What are the risks and costs?”
This isn’t about chasing the newest drug. It’s about finding a treatment that helps you live better-not just survive with diabetes. The options today are better than ever. You just need to know what’s out there.