Dental Implant Candidacy Checker
Select any medical conditions that apply to you. This tool identifies contraindications that may affect implant success.
Not everyone is a good candidate for dental implants. While they’re one of the most reliable ways to replace missing teeth, putting an implant in the wrong person can lead to failure, infection, or even serious health risks. If you’re considering dental implants, it’s not enough to just want them-you need to be medically and physically right for them.
Uncontrolled Diabetes
If you have diabetes that isn’t well-managed, your body struggles to heal properly. High blood sugar slows down tissue repair and weakens your immune response. Studies show that people with HbA1c levels above 8% have a 2-3 times higher risk of implant failure compared to those with levels under 7%. Even if your dentist sees healthy gums, your jawbone may not fuse properly with the implant. Many dentists will refuse to place implants until your blood sugar is stable for at least 3-6 months. This isn’t about being perfect-it’s about giving your body the best shot at healing.
Active Gum Disease
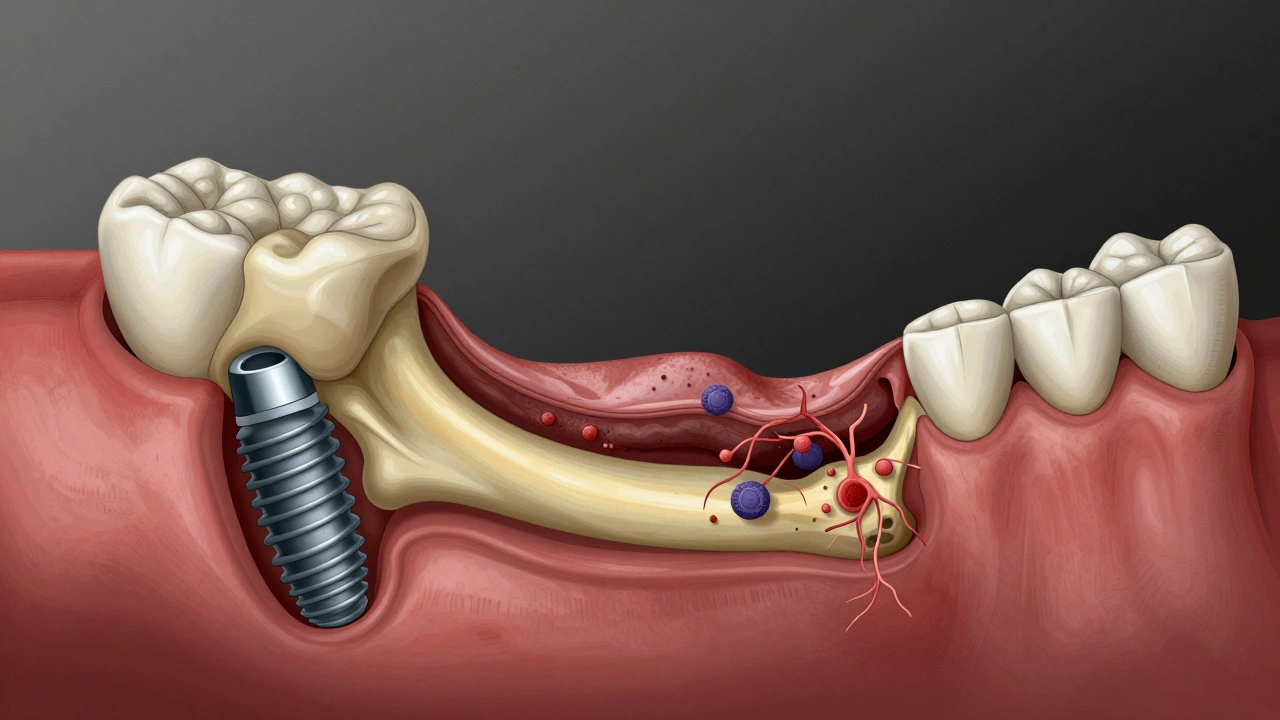
Implants don’t get cavities, but they can still get infected. That infection is called peri-implantitis, and it’s often caused by the same bacteria that cause gum disease. If you still have active periodontitis when you get an implant, the infection will spread to the implant site. The bone around the implant will dissolve, and the implant will loosen. Before any implant is placed, you must have your gums treated and stabilized. This often means deep cleaning, antibiotics, and months of monitoring. Skipping this step is like building a house on sand-no matter how strong the materials, it won’t last.
Severe Bone Loss Without Grafting
Dental implants need solid bone to anchor into. If you’ve lost teeth for years, your jawbone may have shrunk significantly. In some cases, the bone is too thin or too soft to hold an implant. You might think, “Can’t they just force it in?” No. Forcing an implant into weak bone leads to early failure. The solution isn’t always obvious-some people need bone grafts, sinus lifts, or ridge expansions. These are major procedures with their own recovery times and risks. If your dentist says you need grafting, don’t assume it’s a quick fix. Ask how many grafts they’ve done, what success rates they see, and whether you’re a good candidate for the graft itself.
Smoking and Tobacco Use
Smoking isn’t just bad for your lungs-it’s a death sentence for dental implants. Nicotine reduces blood flow to your gums and jawbone. That means less oxygen, fewer healing cells, and slower recovery. Studies show smokers have up to a 20% higher failure rate than non-smokers. The risk goes up with every cigarette. Heavy smokers (more than 10 a day) often have failure rates above 30%. Even if you quit the day before surgery, the damage from past smoking lingers for months. Many clinics won’t place implants unless you’ve been tobacco-free for at least 8 weeks. Some require 3-6 months. If you’re serious about implants, quitting isn’t optional-it’s part of the treatment plan.
History of Radiation Therapy to the Head or Neck
If you’ve had radiation for head or neck cancer, your jawbone changes permanently. Radiation kills blood vessels and reduces the bone’s ability to regenerate. This condition is called osteoradionecrosis. Implants in radiated bone have a failure rate of 30-50%, far higher than in healthy bone. Some patients still get implants, but only after careful evaluation by a specialist. You’ll need advanced imaging, blood flow tests, and often hyperbaric oxygen therapy before and after surgery. This isn’t something a general dentist can handle alone. If you’ve had radiation, talk to a maxillofacial surgeon who specializes in reconstructive cases.
Uncontrolled Autoimmune Diseases
Conditions like lupus, rheumatoid arthritis, or Sjögren’s syndrome can interfere with healing. Some medications used to treat these-like corticosteroids or biologics-suppress the immune system. While this helps control the disease, it also makes it harder for your body to integrate the implant. Patients on high-dose steroids (more than 10 mg prednisone daily) have significantly higher failure rates. If you’re on these meds, your dentist will need to coordinate with your rheumatologist. Sometimes, a temporary pause in medication is possible. Other times, implants are simply too risky. Don’t assume your dentist knows your full medical history-bring your medication list and lab results to every appointment.
Severe Bruxism (Teeth Grinding)
If you grind your teeth hard and often, you’re putting extreme pressure on your teeth-and your implants. Implants don’t have a periodontal ligament like natural teeth. That means they can’t absorb shock. All the force goes straight into the bone. Over time, this causes micro-movements, bone loss, and implant fracture. Many patients don’t even realize they grind their teeth until their dentist sees wear on their natural teeth. If you have bruxism, you’ll need a night guard. But even with a guard, some people still put too much stress on implants. In severe cases, dentists recommend alternative options like bridges or removable dentures instead of implants.
Teenagers with Unfinished Jaw Growth
Implants are permanent. Once placed, they don’t move. But if you’re under 18 and your jaw is still growing, the implant will stay in place while your natural bone shifts. This can lead to misalignment, gum recession, or an implant that looks like it’s sinking below the gumline. For boys, jaw growth usually stops around 17-18. For girls, it’s often 15-16. If a teenager gets an implant too early, they’ll likely need revision surgery later. That’s expensive, painful, and avoidable. Orthodontists and dentists will almost always wait until growth is confirmed complete-usually with a hand-wrist X-ray or a second opinion from a specialist.
Pregnancy
While dental implants aren’t dangerous during pregnancy, they’re not recommended. Surgery, anesthesia, and antibiotics carry small risks. Plus, your body is already under stress. Hormonal changes can make your gums more sensitive and prone to swelling. If you need a tooth replaced, temporary solutions like removable partials or bonded bridges are safer. Wait until after delivery and recovery before considering implants. If you’re planning pregnancy, get your dental work done ahead of time. Don’t delay needed treatment, but don’t start major procedures during pregnancy either.

Psychological or Cognitive Conditions That Prevent Proper Care
Dental implants require lifelong maintenance. You need to brush twice a day, floss around the implant, and visit your dentist every 6 months. If you have dementia, severe anxiety, or uncontrolled mental health conditions that make consistent oral hygiene impossible, implants are not the right choice. An implant that isn’t cleaned properly will fail. And if you can’t follow up with appointments, problems won’t be caught early. In these cases, removable dentures or other low-maintenance options are safer and more realistic. It’s not about ability-it’s about sustainability.
Financial or Lifestyle Factors That Prevent Follow-Up
Implants aren’t just a one-time cost. You need regular check-ups, professional cleanings, and occasional repairs. If you can’t afford ongoing care or don’t have access to a dentist nearby, you’re setting yourself up for failure. Many people get implants and then disappear for years. When they come back, the implant is loose or infected. At that point, it’s too late to save it. If you’re unsure you can commit to long-term care, talk to your dentist about alternatives. A well-fitted denture is better than a failed implant.
What If You’re Not a Candidate?
Not being a candidate for implants doesn’t mean you’re out of options. Removable partial dentures, fixed bridges, or even full dentures can restore function and appearance. Advances in materials mean today’s dentures look and feel more natural than ever. Some people use implant-supported overdentures-where just 2-4 implants hold a full arch in place. That’s often more affordable and less risky than individual implants. The goal isn’t to get the most expensive solution-it’s to get the one that works for your body, your health, and your lifestyle.
Can I get dental implants if I have high blood pressure?
Yes, if your blood pressure is controlled with medication. Uncontrolled hypertension increases bleeding risk during surgery and slows healing. Your dentist will check your blood pressure before the procedure. If it’s too high, they’ll reschedule until it’s stable. Most patients on standard blood pressure meds have no issues with implants.
Are dental implants safe for older adults?
Age alone doesn’t disqualify you. Many people in their 70s and 80s get implants successfully. What matters more is overall health, bone quality, and ability to maintain oral hygiene. If you’re active, eat well, and can brush and floss, implants are a great option-even with age-related bone loss, grafting can help.
Can I get implants if I take blood thinners?
Usually yes, but it requires coordination. Blood thinners like warfarin or apixaban increase bleeding risk. Most dentists won’t ask you to stop them-you’re at higher risk for a stroke or clot if you do. Instead, they’ll use techniques like sutures, hemostatic agents, and careful surgical planning to minimize bleeding. Always tell your dentist exactly what medications you’re on.
Do cancer patients ever get dental implants?
Some do, but only after treatment ends and with specialist approval. If you’ve had chemotherapy or radiation, your body’s healing ability is compromised. Implants are typically delayed for at least 6-12 months after treatment. You’ll need a thorough evaluation by both your oncologist and a maxillofacial surgeon. Success is possible, but it’s not guaranteed.
What if I only have one missing tooth-can I still be denied an implant?
Yes. Even for a single tooth, your overall health matters more than how many teeth are missing. If you have uncontrolled diabetes, smoke heavily, or have poor bone quality, your dentist may recommend a bridge or other option instead. One implant isn’t worth the risk if the chance of failure is high.
Next Steps If You’re Unsure
Don’t guess whether you’re a candidate. Get a full evaluation. That means X-rays, a 3D scan (CBCT), a gum health check, and a full medical history review. Ask your dentist: “What’s the biggest risk for me?” and “What would you do if this was your family member?” If they push you toward implants without addressing your health concerns, get a second opinion. The best implant dentist isn’t the one who places the most implants-it’s the one who tells you when not to get them.
