Wegovy Prior Authorization Checker
Results
Getting Express Scripts to approve Wegovy isn’t about luck-it’s about paperwork, timing, and knowing exactly what they’re looking for. If you’ve been prescribed Wegovy for weight loss and your pharmacy says it’s denied, don’t panic. Thousands of people face this exact roadblock every month. The issue isn’t that Wegovy doesn’t work-it’s that insurance companies like Express Scripts have strict rules before they’ll pay for it.
Why Express Scripts Denies Wegovy Claims
Express Scripts, which manages prescriptions for over 90 million people in the U.S., doesn’t deny Wegovy because it’s expensive (though it is). They deny it because of their own internal guidelines. These aren’t random-they’re based on CDC and FDA recommendations for obesity treatment. Here’s what they check first:- Your BMI must be 30 or higher (obesity), or 27 or higher with at least one weight-related condition like high blood pressure, type 2 diabetes, or sleep apnea.
- You must have tried and failed other weight loss methods-usually documented diet and exercise programs over 3-6 months.
- Your doctor must prove Wegovy isn’t just for cosmetic reasons. They need to show it’s medically necessary.
- You can’t be taking other GLP-1 drugs like Ozempic or Saxenda at the same time.
What Your Doctor Needs to Submit
The biggest mistake people make? Assuming their doctor knows what Express Scripts wants. Most doctors don’t. They write a standard prescription and assume that’s enough. It’s not. Your doctor needs to submit a prior authorization request that includes:- Your full medical history-especially any obesity-related conditions (diabetes, hypertension, fatty liver, etc.)
- Proof of prior weight loss attempts: diet logs, gym records, or notes from nutritionists
- Lab results from the last 6 months: HbA1c, cholesterol, liver enzymes
- A signed statement: "Wegovy is medically necessary for treatment of obesity and associated comorbidities. Alternative treatments have failed."
- E66.9 - Unspecified obesity
- E11.9 - Type 2 diabetes without complications
- I10 - Essential (primary) hypertension
How to Follow Up Without Getting Ignored
After your doctor submits the request, don’t wait. Call Express Scripts directly. Use the number on the back of your insurance card. Ask for the Prior Authorization Department, not customer service. When you call, have ready:- Your member ID
- Your doctor’s name and NPI number
- The date the request was submitted
- A reference number if they gave you one
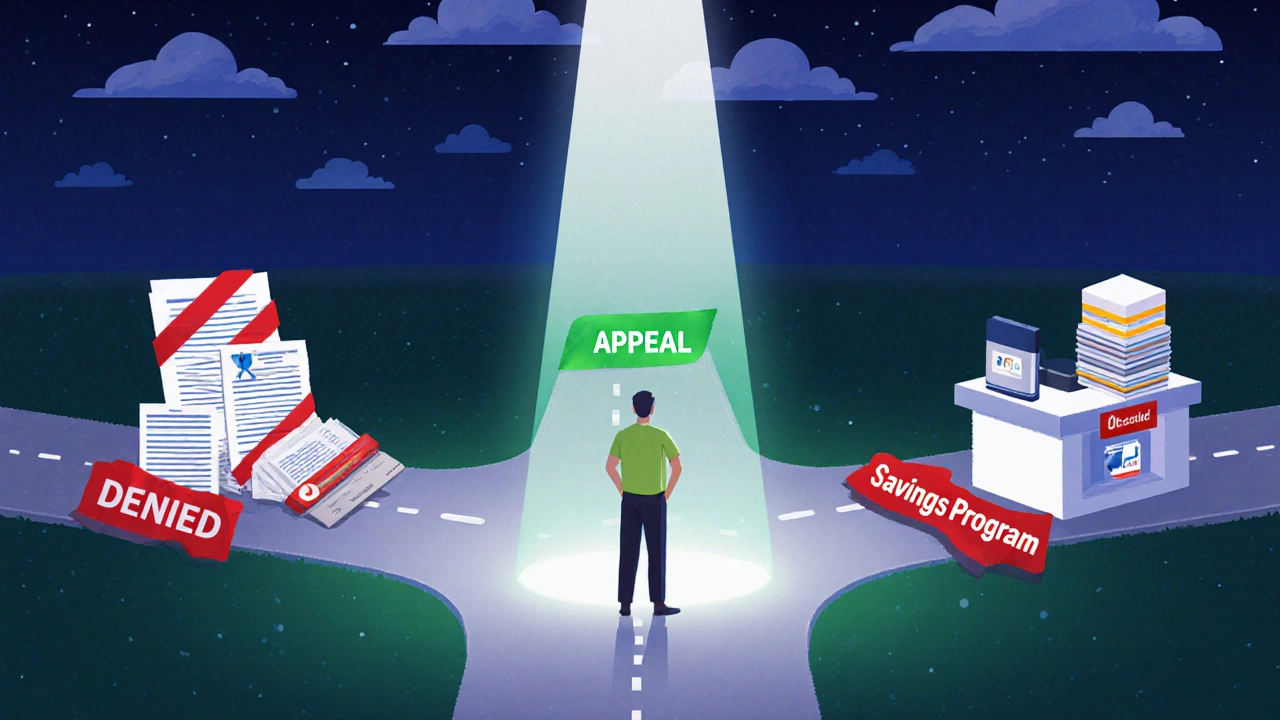
What to Do If It’s Denied
If you get a denial letter, don’t accept it as final. You have 60 days to appeal. The appeal letter must include:- A copy of the denial letter
- Updated medical records showing your condition hasn’t improved
- A letter from your doctor explaining why Wegovy is the best option-especially if you’ve tried metformin, liraglutide, or orlistat before
- Any recent weight measurements (even if it’s just 5 pounds lost)
Alternative Paths If Approval Still Fails
If Express Scripts still says no after two tries, you have options:- Wegovy Savings Card: Eligible patients can pay as low as $25 per month through the manufacturer’s program. You still need a prescription, but you don’t need insurance.
- Pharmacy discount programs: Some independent pharmacies offer Wegovy at wholesale prices-sometimes under $400/month without insurance.
- Health Savings Account (HSA) or FSA: You can use pre-tax dollars to pay for Wegovy if you have one. Many people don’t realize this is allowed.
- Switch insurers: Some Medicare Advantage plans or employer plans have better coverage for GLP-1s. If you’re changing jobs or open enrollment is near, this might be worth considering.
Common Mistakes That Cost People Approval
Here’s what goes wrong more often than you’d think:- Using "overweight" instead of "obesity" in documentation. Express Scripts doesn’t cover overweight-they cover obesity.
- Not including lab results. A BMI alone isn’t enough. They want proof your body is struggling.
- Waiting too long to follow up. The system takes 7-14 days. If you wait 3 weeks, you miss the window.
- Letting your doctor submit it as a "specialty drug" without prior auth. That’s a guaranteed denial.
- Trying to use a mail-order pharmacy that doesn’t work with Express Scripts. Stick to in-network pharmacies.
How Long Does Approval Take?
Typically, it takes 3-10 business days after your doctor submits the request. If you follow up on day 5, you’ll often get a decision by day 7. Expedited reviews are possible if you have severe comorbidities-like uncontrolled diabetes or heart disease. Just ask your doctor to mark it as "urgent."Final Tip: Keep Records
Always save copies of:- Every denial letter
- Doctor’s notes
- Lab reports
- Call logs with dates and names of reps you spoke to
Wegovy isn’t a magic pill. It’s a tool. But it only works if you can get it. The system is stacked against you-but not unbeatable. With the right documentation, persistence, and a few smart moves, you can get approved.
Can I get Wegovy without insurance through Express Scripts?
No, Express Scripts is an insurance pharmacy benefit manager. If you don’t have insurance, they won’t process your claim. But you can still get Wegovy through the manufacturer’s savings program or at select pharmacies that offer cash pricing. You don’t need Express Scripts to fill the prescription-you just need a valid prescription from your doctor.
How long do I need to be on a diet before Express Scripts approves Wegovy?
There’s no set time, but most approvals require documentation of at least 3-6 months of documented lifestyle changes. This could be a nutrition program, gym attendance logs, or notes from a weight loss coach. The key is showing you tried before turning to medication.
Does Express Scripts cover Wegovy for prediabetes?
Yes-if you have a diagnosis of prediabetes (ICD-10 code R73.03) and a BMI of 27 or higher. Prediabetes counts as a weight-related condition under their guidelines. Make sure your doctor codes it correctly and includes your HbA1c level in the prior authorization request.
Can I switch from Ozempic to Wegovy and get approval?
Yes, but only if you’ve tried Ozempic for at least 3 months and it didn’t work-or you couldn’t tolerate the side effects. Express Scripts requires proof of failure with other GLP-1s before approving Wegovy. Your doctor must document this clearly in the prior auth request.
What if my doctor won’t help with the prior authorization?
If your doctor refuses, ask for a referral to an endocrinologist or obesity medicine specialist. These providers are more familiar with insurance requirements. Some telehealth clinics specialize in weight loss medications and handle prior authorizations for you. You can also contact the Wegovy manufacturer’s support line-they’ll connect you with a patient advocate who can help guide your doctor through the process.