Survival Rates: What They Really Mean for Your Health Decisions
When you hear survival rates, the percentage of people alive after a certain time following a diagnosis or treatment, it’s easy to think it’s a simple yes-or-no answer. But survival rates aren’t predictions for you—they’re averages pulled from thousands of people with similar conditions. These numbers help doctors compare treatments, but they don’t tell you if you’ll be in the 70% who make it or the 30% who don’t. What matters more is how those rates were measured: were they based on people who got early treatment? Did they include those with other health problems? The same cancer might have a 60% five-year survival rate in one study and 75% in another, simply because the groups were different.
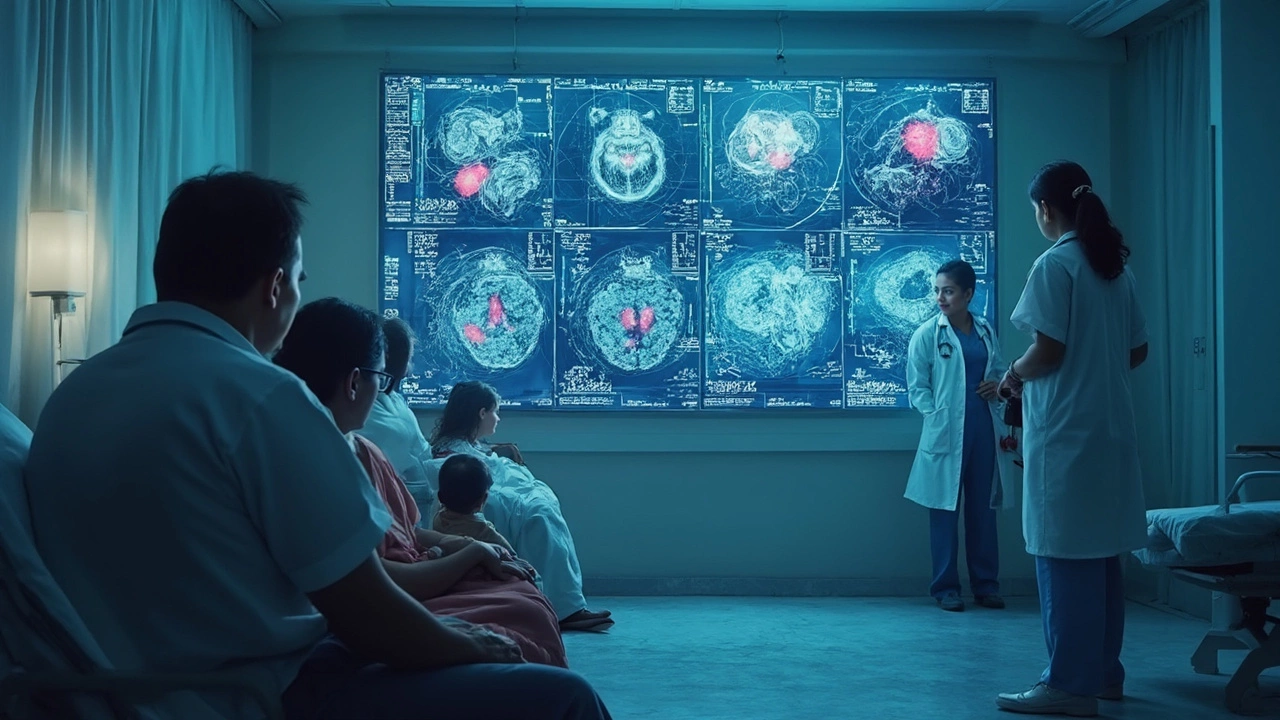
Health outcomes, the real-world results of medical care like how long someone lives or how well they function after treatment are what actually shape your life. A high survival rate doesn’t mean you’ll feel good during treatment. Someone might survive five years with stage 3 lung cancer but spend most of that time in pain, on oxygen, or unable to work. That’s why survival rates need to be paired with treatment success, how well a therapy works at stopping disease progression or improving daily life. For example, a diabetes drug might have a 90% survival rate over ten years, but if it causes constant nausea or weight gain, is it really a success for you? And then there’s medical prognosis, a doctor’s best guess about how your condition will progress based on your age, other illnesses, and test results. This isn’t a number you find online—it’s a conversation you have with your doctor after reviewing your blood work, scans, and lifestyle.
Look at the posts here. You’ll see real examples: people asking if they’re good candidates for knee replacements, whether IVF leads to twins, or if new diabetes drugs like tirzepatide actually improve long-term survival. These aren’t abstract stats—they’re personal decisions wrapped in data. Survival rates are tools, not verdicts. They help you ask better questions: What’s the quality of life during treatment? How many people dropped out because of side effects? Did the study include people like me? The answers aren’t in one number. They’re scattered across studies, doctor notes, and real stories from people who’ve been there. What follows isn’t just a list of articles—it’s a collection of real-life contexts that turn cold numbers into human choices.

Has Anyone Survived Stage 4 Cancer? Real Stories and What Science Says
•13 Jan 2026
Many people survive stage 4 cancer today thanks to advances in targeted therapy, immunotherapy, and personalized treatment. Real patients are living years-sometimes decades-with stable, manageable disease.
Hardest Cancer to Cure: What Makes Treatment So Tough?
•29 Apr 2025
Not all cancers act the same—some are much tougher to treat than others. This article digs into which cancer is the hardest to cure and why it's so stubborn. You'll learn what makes these cancers aggressive, how doctors are fighting back, and what signs to watch for. It covers new treatment options and small things people can do right now to boost their odds. Get the details on why early detection matters and what's on the horizon.